What are Implants / Transcervical Sterilization?
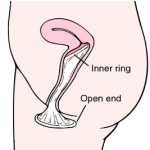
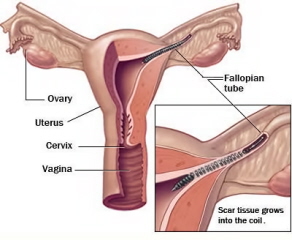
When the word “transcervical” (meaning “through the cervix“) sterilization is used, it’s meant to encompass any method of Permanent Contraception where a health care provider reaches the fallopian tubes through the cervical opening of the uterus to block the tubes, preventing an unintended pregnancy.
In 2002 the U.S. Food and Drug Admisitration (FDA) approved a small metallic implant called Essure as safe form of Permanent Contraception. The implant itself is a small, soft, flexible metal and fiber coil that is placed into the fallopian tubes to prevent pregnancy.
How does a the Essure Implant work?
Once the Essure Implants are in place it works by making scar tissue form over the implant, blocking the fallopian tube and preventing fertilization of the egg by the sperm.
 How is a Transcervical Sterilization performed?
How is a Transcervical Sterilization performed?
The procedure does not require cutting into the body or the use of radio frequency energy to burn the fallopian tubes. Instead, a health care professional inserts the soft, flexible implants through the body’s natural pathways (vagina, cervix, and uterus) and places one into the opening of each of the 2 fallopian tubes. The very tip of the device remains outside the fallopian tube, which provides immediate visual confirmation that it is in place.
What can a patient expect after the procedure?
During the 3 months following the procedure, the patients body forms scar tissue over the inserts to form a natural barrier that prevents sperm from reaching the egg. During this period, the patient must continue using another form of birth control like a condom.
After three months, it’s time to get a confirmation test to verify that the patient is protected from the possibility of an unplanned pregnancy. The test uses a dye and special type of x-ray to ensure both that the inserts are in place and that the fallopian tubes are completely blocked.
What are the advantages?
- No surgery, burning or anesthesia
- No hormones
- No slowing down to recover
- Can be performed in less than 30 minutes
- Allows sexual spontaneity and requires no daily attention.
- It is a permanent form of birth control.
- There are no changes in sexual desire, menstrual cycle, or ability to breastfeed
- May be covered by Heath Insurance
What are the disadvantages?
- May not be reversible.
- It is meant to be a permanent form of birth control, and some women may regret the decision later.
- The two most common factors associated with regret are young age and unpredictable life events, such as change in marital status or death of a child.
- It can be expensive, usually around $2,000 with insurance covering a portion
- Allergic reaction to the materials
- Perforation, expulsion, or other unsatisfactory location of the micro-insert
- Symptoms during or immediately after the procedure may include mild to moderate cramping, nausea/vomiting, dizziness/light-headedness, and bleeding/spotting
- Not all women will achieve successful placement of both inserts
How effective is the Essure Implant/Transcervical Sterilization?
During clinical trials the Essure procedure was found to be 99.74% effective.
Stay up to date with Sex Ed 102: Just sign up for an email update through the form below!


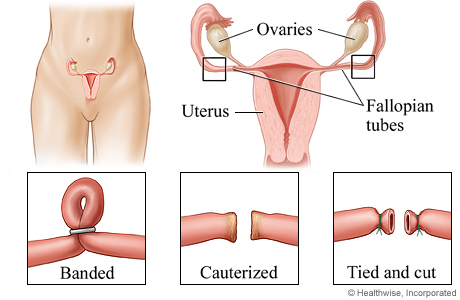
 How is a Tubal Ligation Performed?
How is a Tubal Ligation Performed?
 What are Condoms?
What are Condoms?